Don't miss
Hallway Huddle
- Chronic kidney disease in type 2 diabetes
14 years ago
·
#44
Accepted Answer
This is a very commonly asked question.
The answer is not entirely known but over the past several years we've had some insights into it. Over time with accumulation of data from clinical trials, it's fairly clear that ACE inhibitors have a greater quantity of data in patients with heart failure had established coronary artery disease in terms of their role in cardioprotection. And so, most contemporary guidelines will position ACE inhibitors ahead of angiotensin receptor blockers for the management of hypertension and to confer cardioprotection in this patient population. Because of studies like ONTARGET and VALIANT, angiotensin receptor blockers have been increasingly viewed as similar if not superior to ACE inhibitors in terms of cardioprotection. In terms of patients with chronic kidney disease particularly due to diabetes, angiotensin receptor blockers have long been associated with preservation of renal function. Of course, these patients are also at risk for cardiovascular disease and so there was temptation to preferentially use ACE inhibitors in this group as well. Once again, now that we have studies such as, ONTARGET and VALIANT, treating patients who have chronic kidney disease with angiotensin receptor blockers is particularly attractive because of the low incidence of side effects with these medications and because these studies have suggested that the cardioprotection seen with ACE inhibitors also applies to this drug class.
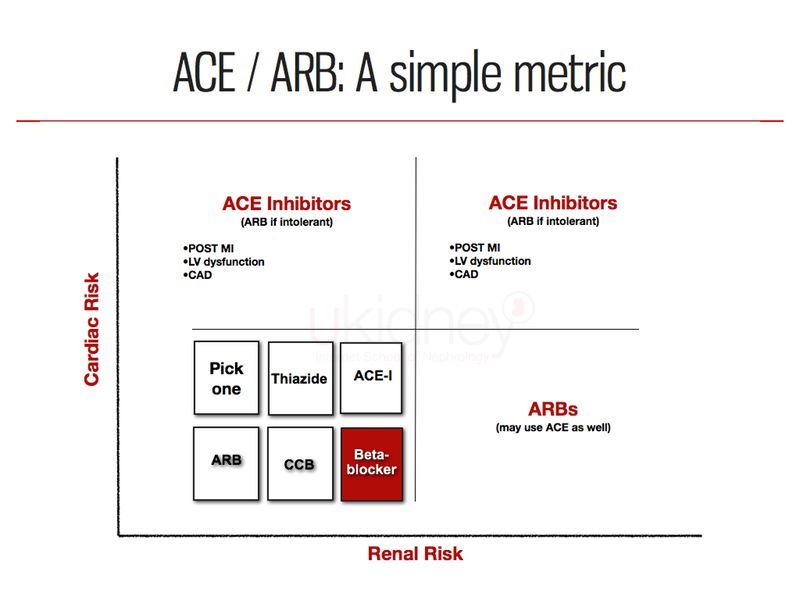
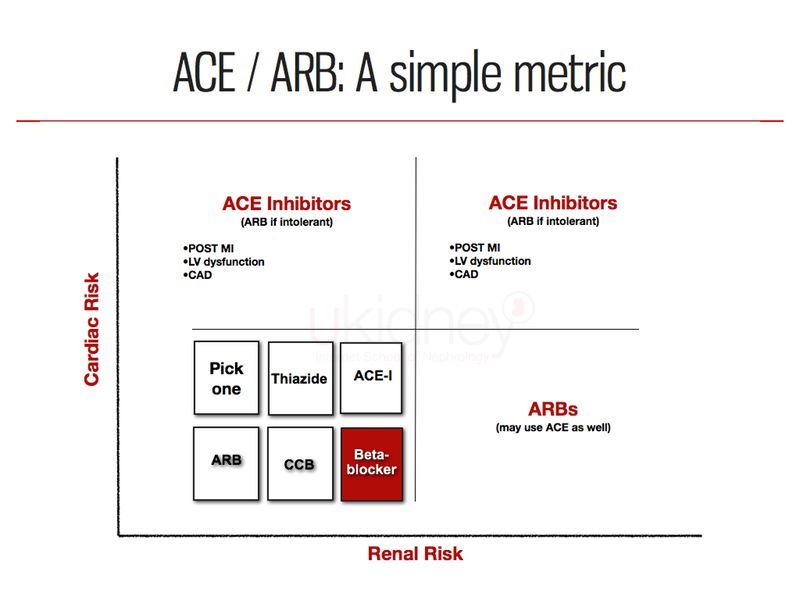
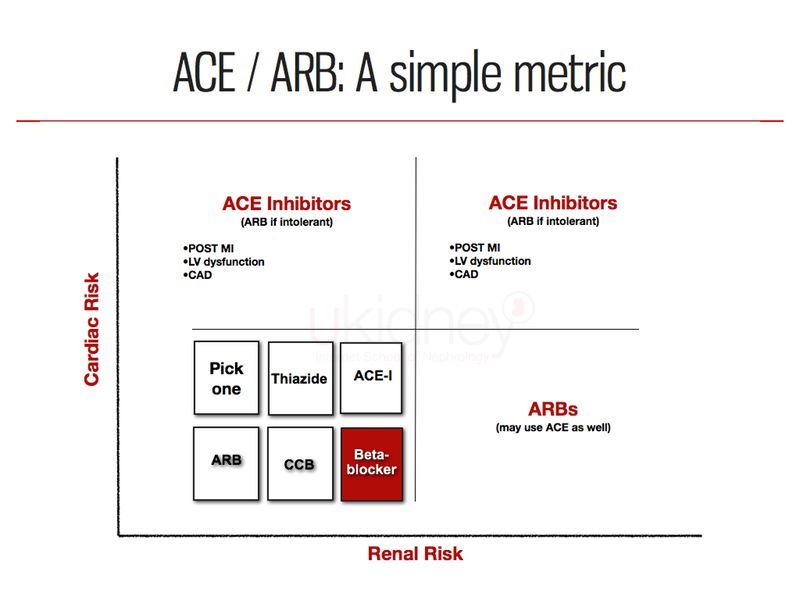
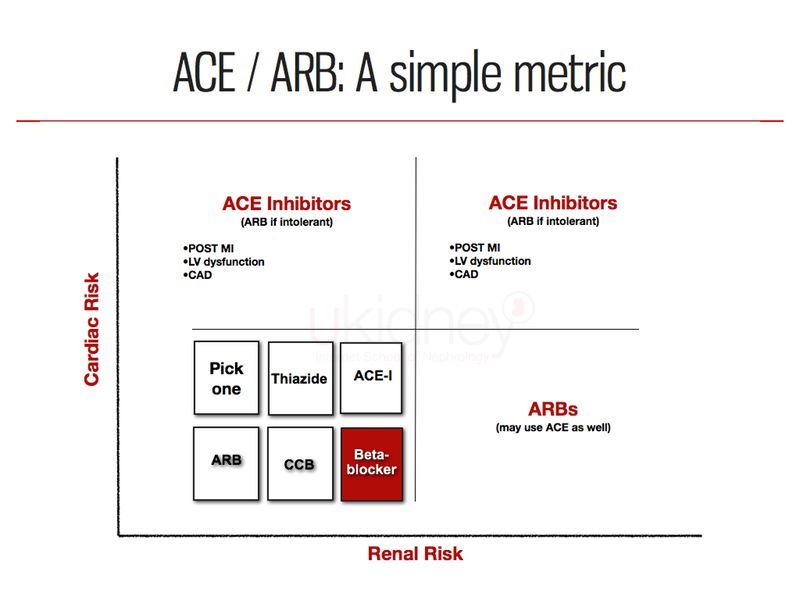
Therefore, in my own practice I actually adopt both medications and use them in an evidence-based fashion depending on the comorbidities. So in patients with primarily cardiovascular disease, without renal disease, I tend to use ACE inhibitors and in those patients without a great burden of cardiovascular disease but more significant renal disease (particularly diabetic renal disease), I tend to use angiotensin receptor blockers 1st in these patients. This practice can be depicted in the figure below:
The answer is not entirely known but over the past several years we've had some insights into it. Over time with accumulation of data from clinical trials, it's fairly clear that ACE inhibitors have a greater quantity of data in patients with heart failure had established coronary artery disease in terms of their role in cardioprotection. And so, most contemporary guidelines will position ACE inhibitors ahead of angiotensin receptor blockers for the management of hypertension and to confer cardioprotection in this patient population. Because of studies like ONTARGET and VALIANT, angiotensin receptor blockers have been increasingly viewed as similar if not superior to ACE inhibitors in terms of cardioprotection. In terms of patients with chronic kidney disease particularly due to diabetes, angiotensin receptor blockers have long been associated with preservation of renal function. Of course, these patients are also at risk for cardiovascular disease and so there was temptation to preferentially use ACE inhibitors in this group as well. Once again, now that we have studies such as, ONTARGET and VALIANT, treating patients who have chronic kidney disease with angiotensin receptor blockers is particularly attractive because of the low incidence of side effects with these medications and because these studies have suggested that the cardioprotection seen with ACE inhibitors also applies to this drug class.
Therefore, in my own practice I actually adopt both medications and use them in an evidence-based fashion depending on the comorbidities. So in patients with primarily cardiovascular disease, without renal disease, I tend to use ACE inhibitors and in those patients without a great burden of cardiovascular disease but more significant renal disease (particularly diabetic renal disease), I tend to use angiotensin receptor blockers 1st in these patients. This practice can be depicted in the figure below:
14 years ago
·
#44
Accepted Answer
This is a very commonly asked question.
The answer is not entirely known but over the past several years we've had some insights into it. Over time with accumulation of data from clinical trials, it's fairly clear that ACE inhibitors have a greater quantity of data in patients with heart failure had established coronary artery disease in terms of their role in cardioprotection. And so, most contemporary guidelines will position ACE inhibitors ahead of angiotensin receptor blockers for the management of hypertension and to confer cardioprotection in this patient population. Because of studies like ONTARGET and VALIANT, angiotensin receptor blockers have been increasingly viewed as similar if not superior to ACE inhibitors in terms of cardioprotection. In terms of patients with chronic kidney disease particularly due to diabetes, angiotensin receptor blockers have long been associated with preservation of renal function. Of course, these patients are also at risk for cardiovascular disease and so there was temptation to preferentially use ACE inhibitors in this group as well. Once again, now that we have studies such as, ONTARGET and VALIANT, treating patients who have chronic kidney disease with angiotensin receptor blockers is particularly attractive because of the low incidence of side effects with these medications and because these studies have suggested that the cardioprotection seen with ACE inhibitors also applies to this drug class.
Therefore, in my own practice I actually adopt both medications and use them in an evidence-based fashion depending on the comorbidities. So in patients with primarily cardiovascular disease, without renal disease, I tend to use ACE inhibitors and in those patients without a great burden of cardiovascular disease but more significant renal disease (particularly diabetic renal disease), I tend to use angiotensin receptor blockers 1st in these patients. This practice can be depicted in the figure below:
The answer is not entirely known but over the past several years we've had some insights into it. Over time with accumulation of data from clinical trials, it's fairly clear that ACE inhibitors have a greater quantity of data in patients with heart failure had established coronary artery disease in terms of their role in cardioprotection. And so, most contemporary guidelines will position ACE inhibitors ahead of angiotensin receptor blockers for the management of hypertension and to confer cardioprotection in this patient population. Because of studies like ONTARGET and VALIANT, angiotensin receptor blockers have been increasingly viewed as similar if not superior to ACE inhibitors in terms of cardioprotection. In terms of patients with chronic kidney disease particularly due to diabetes, angiotensin receptor blockers have long been associated with preservation of renal function. Of course, these patients are also at risk for cardiovascular disease and so there was temptation to preferentially use ACE inhibitors in this group as well. Once again, now that we have studies such as, ONTARGET and VALIANT, treating patients who have chronic kidney disease with angiotensin receptor blockers is particularly attractive because of the low incidence of side effects with these medications and because these studies have suggested that the cardioprotection seen with ACE inhibitors also applies to this drug class.
Therefore, in my own practice I actually adopt both medications and use them in an evidence-based fashion depending on the comorbidities. So in patients with primarily cardiovascular disease, without renal disease, I tend to use ACE inhibitors and in those patients without a great burden of cardiovascular disease but more significant renal disease (particularly diabetic renal disease), I tend to use angiotensin receptor blockers 1st in these patients. This practice can be depicted in the figure below:
14 years ago
·
#47
Hi Dr. Weinstein…. I like your argument very much … I used the same rule to choose between both drugs..Beside most of ACEi needed dose adjust depending on GFR .. None of the ARB needed it … but how about renine direct inhibitors? When do you use it if you are using it at all?
14 years ago
·
#48
Hello,
The best answer to your question will come when the ALTITUDE and ASTRONAUT studies are completed. In the meantime, I believe the role for DRI is to add on to ACEi or ARB for lowering BP, particularly in patients with elevated albumin excretion. The DRI class can also be used in the absence of albuminuria as add-on to ACEi or ARB but their use is especially important when albuminuria persists.
I believe that the use of DRI-based combinations will eventually prove to be distinctly different from ACE/ARB combinations since the latter raise plasma renin activity (PRA) reflexively whereas DRI obviously lower PRA. And we have known for some time that PRA elevation is associated with adverse cardiovascular outcomes.
The best answer to your question will come when the ALTITUDE and ASTRONAUT studies are completed. In the meantime, I believe the role for DRI is to add on to ACEi or ARB for lowering BP, particularly in patients with elevated albumin excretion. The DRI class can also be used in the absence of albuminuria as add-on to ACEi or ARB but their use is especially important when albuminuria persists.
I believe that the use of DRI-based combinations will eventually prove to be distinctly different from ACE/ARB combinations since the latter raise plasma renin activity (PRA) reflexively whereas DRI obviously lower PRA. And we have known for some time that PRA elevation is associated with adverse cardiovascular outcomes.
14 years ago
·
#67
Dr. Weinstein,
This is a very clear explanation of this difficult question. Couldn't one make things simpler though by just prescribing ACE OR ARB to all patients and not distinguishing?
This is a very clear explanation of this difficult question. Couldn't one make things simpler though by just prescribing ACE OR ARB to all patients and not distinguishing?
14 years ago
·
#78
@drshahir my short answer is no.
I will create a new question specifically to address this.
I will create a new question specifically to address this.
14 years ago
·
#79
@Nidia Pernalete
This is a very surprising. Just announced today, but it seems the role of DRI added on to ACE or ARB has been dealt a large blow:
BREAKING: No benefit of Aliskiren added on to ACEi or ARB. ALTITUDE study halted (LINK: http://ukid.cc/tAXLRp)
This is a very surprising. Just announced today, but it seems the role of DRI added on to ACE or ARB has been dealt a large blow:
BREAKING: No benefit of Aliskiren added on to ACEi or ARB. ALTITUDE study halted (LINK: http://ukid.cc/tAXLRp)
- Page :
- 1
There are no replies made for this post yet.

LEADING RESOURCE IN NEPHROLOGY EDUCATION