UKidney Nephrology News and Insights
Hypertension targets following the SPRINT study
Welcome to the Circle of Knowledge Program
Two Canadian experts, Dr. Jordan Weinstein and Dr. Louis Girard, nephrologists, will share how to translate clinical evidence into daily practice for optimal hypertension patient care.
Hypertension is one of the most important risk factors for adverse health outcomes that we treat either in specialty or primary care. However, controversy has always existed in terms of the target blood pressure that clinicians should aim for when managing patients with different comorbidities. The SPRINT study published in 2015 continues to offer insight and some controversy guiding therapy in patients with hypertension particularly those at high cardiovascular risk.
This landmark trial enrolled 9361 non-diabetic patients over age 50 at high cardiovascular risk but excluded those with prior stroke, frail elderly or those patients with protein excretion > 1g per day. Participants were randomized to either a blood pressure target <140 mmHg or <120 mmHg. For the purpose of this trial, the definition of cardiovascular risk required a history one or more of the following:
- clinical or subclinical cardiovascular disease other than stroke;
- chronic kidney disease, excluding polycystic kidney disease, with an estimated glomerular filtration rate (eGFR) of 20 to less than 60 ml per minute per 1.73 m2
- a 10-year risk of cardiovascular disease of 15% or greater on the basis of the Framingham risk score;
- 75 years or older. Patients with diabetes mellitus or prior stroke were excluded
Patients achieved mean systolic blood pressures of 121.5 and 134.6 using automated oscillometric blood pressure (AOBP) and the intensively treated patients required on average approximately 2.8 blood pressure lowering medications as compared with 1.8 medications in the standard treatment group.
Primary outcome of the trial was a composite of:
- myocardial infarction
- acute coronary syndrome
- stroke
- acute decompensated heart failure
- cardiovascular death.
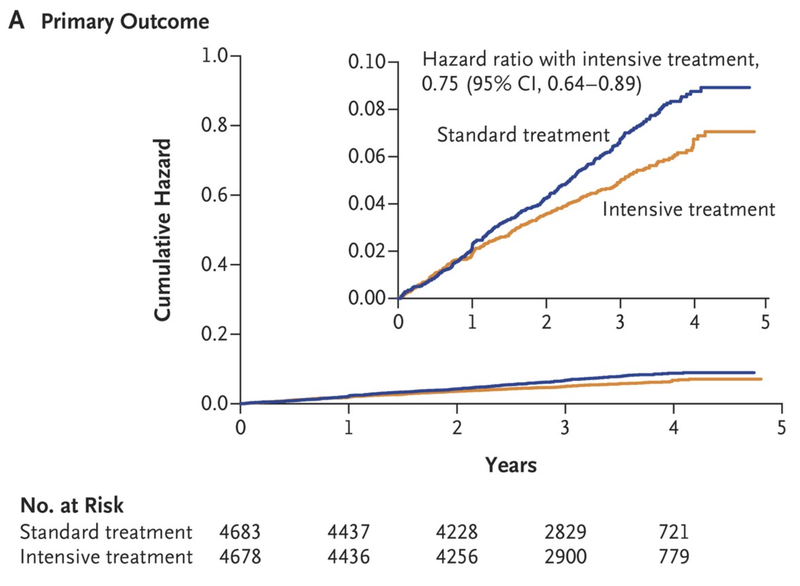
Investigators stopped the trial three years into a planned five year study on the basis of a significantly lower rate of the primary outcome and all-cause mortality in the intensively treated group. The observed benefit came at the expense of hypotension, syncope, electrolyte abnormalities and acute kidney injury or acute renal failure in the intensively treated group but injurious falls were not significantly increased.
While the study and its outcomes can be debated for a variety of methodologic details, it likely will inform the target blood pressure for patients at high cardiovascular risk moving forward. Therefore, if patients do meet the SPRINT enrollment criteria, after a discussion of the risks and benefits, clinicians should consider prescribing a target of 125 to 130 mmHg if using a manual blood pressure measurement and 120 to 125 mmHg when using AOBP. The recommended BP target is based on achieved blood pressures in SPRINT, even though the study protocol aimed for <120 mmHg.
Of course, SPRINT did not address the important sub groups such as those with diabetes and or prior history of stroke; nor does the SPRINT study inform us about patients with proteinuric chronic kidney disease (> 1g per day of protein excretion) or the frail elderly. These important subgroups will be the subject of a future post in the Circle of Knowledge series.
Monthly Clinical Pearl
In patients at high cardiovascular risk, providers should aim for a blood pressure range of 125 to 130 mmHg if using a manual blood pressure measurement and 120 to 125 mmHg when using AOBP.
High cardiovascular risk can defined as:
- clinical or subclinical cardiovascular disease other than stroke;
- chronic kidney disease, excluding polycystic kidney disease, with an estimated glomerular filtration rate (eGFR) of 20 to less than 60 ml per minute per 1.73 m2
- a 10-year risk of cardiovascular disease of 15% or greater on the basis of the Framingham risk score;
- 75 years or older. Patients with diabetes mellitus or prior stroke were excluded